It may surprise many of you to know that some vaccines currently being used are actually composed of a living virus that actively replicates in your body in order to generate immunity. I’ve written about one of these live vaccines before on this site: the oral polio vaccine (OPV). These are effective vaccines that mount a long-term adaptive immunity to the pathogen in question. This is done by immune cells that break down the virus and present small parts known as antigens to immature immune cells, which then mature in response to the antigen and are then capable of mounting an immune response to this same challenge in the future.
A recent paper to come out has shown one way that these live but attenuated viruses can be capable of generating such an effective immune response in vivo. Read on to see a potentially novel mechanism in generating an adaptive immune response to cytopathic viruses.
I almost titled this article “Things the spleen can do for you” because of the interesting mechanism that was demonstrated in a recent paper in Nature Immunology. In this study, Honke et al used the vesicular stomatitis virus (VSV) to show that a subset of immune cells selectively and locally lower the initial innate immune response in order to permit viral replication in a discreet region of the spleen known as the marginal zone (Fig1 Ludewig and Cervantes-Barragan). Here, only CD169+ macrophages are actively infected with VSV (CD169+ refers to a type of protein found on the cellular surface that makes them unique). These macrophages then present small broken up parts of the virus called antigens to immature B cells in the white pulp of the spleen, another type of immune cell. These B cells respond to the antigen presented by the macrophage and then begin to generate antibodies to these very fragments, which provide effective protection to future challenges by the same pathogen.

Presentation of antigen to B cells is a normal part of the adaptive immune response, but what is special here is the fact that a specific subset of macrophages called CD169+ macrophages are responsible for this enforced viral replication in the marginal zone of the spleen in order to generate enough antigen to stimulate nearby immature B cells in the white pulp (Figure 1G Honke et al).

This zone of permissive replication is a unique mechanism because most macrophages, when exposed to a recognizable virus, secrete compounds called interferons. These are strongly-acting antiviral effectors that tell all cells to enter an antiviral program that limits the spread of virus. While this is an effective way of shutting down an early infection, it also limits the amount of replicating virus and the amount of antigen that can be presented to B cells. If immature B cells are not stimulated by antigen they will not mature to produce antibody and you will not develop long-term immunity. In this way it is possible for the innate immune system to shut out an infection before an adaptive immune response can be mounted. This means that while the host has been infected it doesn’t have an immunological “memory” of the pathogen. This leaves only the innate defenses, which can be overcome.
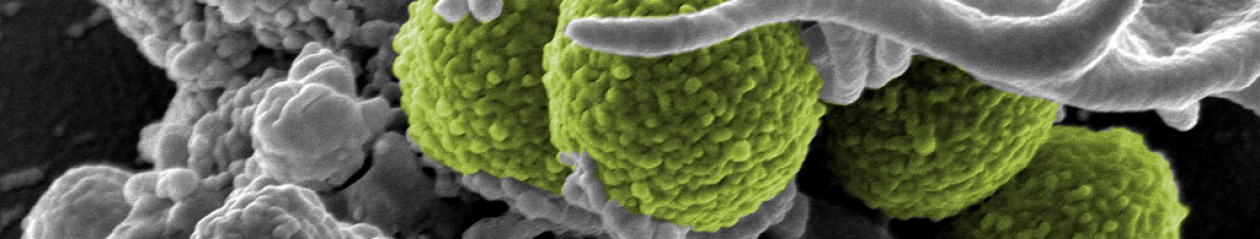
By amplifying some virus in a discreet space in the marginal region of the spleen in these CD169+ macrophages the body are able to create a “backdoor” to prime the adaptive immune response. See Fig1G at right from Honke et al. This marginal region is populated by CD169+ macrophages (red) and replicating VSV (green), but both are absent elsewhere in the imaged splenic sections. The appearance of yellow indicates that these signals are coming from the same location in the marginal zone. (For a more in-depth discussion of why red and green make yellow see my post on Immunoflourescent Microscopy).
This initial containment is critical, as once the virus escapes the innate response it can multiply unchecked unless there is an adaptive response to control it. This was shown in Figure 5B, where mice without this ability to backdoor antigen to B cells died after exposure to VSV, while those that generated the adaptive response were able to survive.

This experiment was done by co-infecting the mice with intravenous VSV, either live or inactivated with UV light, and intranasally them with live VSV. Those mice that had active VSV given by IV were able to generate a faster antibody response and were better able to survive the challenge. Those that were given the UV inactivated virus took longer to generate an antibody response (Fig 5A) and died (Fig 5B) as a result of the virus invading their central nervous systems. It should be noted that all mice were able to develop antibodies to VSV, so this form of antigen amplification and delivery is not a requirement for developing an immune response but it is capable of inducing a faster response.
Hence the compartment of permissive viral replication to control viral growth. This mechanism could be seen as a way to generate antibodies to viruses that replicate fast and can escape innate control before antibodies can be generated in the canonical manner. VSV is one of these viruses: it is an RNA virus in the Rhabdoviridae family, a close relative of Rabies virus with fast growth kinetics. While this is speculative on my part, it could be possible that this is a mechanism employed by higher animals to generate a faster response to certain viruses. This may be dangerous, as allowing the virus to replicate at all may increase chances of escape, but if it were to escape the host needs antibodies to effectively protect itself. A double-edged sword for the host, but potentially life-saving.

Another fascinating aspect of this model is that the enhanced viral replication in these CD169+ macrophages is a direct result of the expression of a protein known as Usp18. This protein works by turning off the interferon response in these macrophages so that they do not enter the antiviral cell program. CD169+ macrophages produce high levels of this protein when infected, this is what allows them to turn off the interferon response and support discrete viral replication in the marginal zone of the spleen. Without Usp18 the macrophages enter the antiviral program dictated by interferon signaling and attempt to control the infection through the innate response. However, by not generating enough antigen to prime the adaptive response these Usp18 knockout mice showed reduced survival and higher levels of VSV neuroinvasion than control mice when VSV escaped innate control (Honke et al Figure 4).
A caveat of this study is that it has only shown this mechanism in play for VSV. The authors do cite data that this also occurred with intravenous infection of LCVM, but the data is not presented. This may be a case specific mechanism, as IV inoculation of high titers of VSV may result in abnormal viral processing (PFU 2 x 10^6, or 2,000,000 viral particles).
As it stands this is an interesting mechanism that may shed light on how the immune system generates immunity to cytopathic viruses. What is exciting about this discovery is that, if it holds for various different pathogens, it could give us new tools and approaches when attempting to design the next generation of live-attenuated viral vaccines. This is critical, as the development of effective vaccines has been one of the biggest contributions to public health in the last century and continues to be the front line in the unending battle between humans and infectious diseases. It will be exciting to see what developments come from this line of research in the next few years, as there is the potential to inform vaccine design with this body of knowledge if the mechanism holds true under further investigation.
Works Referenced:
1. Honke, N. et al. Enforced viral replication activates adaptive immunity and is essential for the control of a cytopathic virus. Nature immunology 13, 51–7 (2012). Figures Used: 1G, 4, 5
2. Ludewig, B. & Cervantes-Barragan, L. CD169+ macrophages take the bullet. Nature immunology 13, 13–4 (2012). Figures used: 1